 Ampicillin Resistance: Causes, Trends, and Prevention Strategies
Ampicillin Resistance: Causes, Trends, and Prevention Strategies
How Misuse of Antibiotics Fuels Resistance 🔥
Clinicians and patients often favor quick fixes, prompting antibiotics for viral infections or stopped courses as symptoms ease. This behavior creates survival pressure: susceptible bacteria die while resistant mutants thrive and multiply, leading to an increasing occurence of hard-to-treat strains in hospitals and the community.
Unchecked use on farms, self-medication, and lax prescribing amplify spread across borders; mobile people and food trade accelerate dissemination globally. Urgent measures, stewardship, rapid diagnostics, public education and regulated veterinary practices can slow selection, preserve existing drugs and protect future patients from dwindling treatment options.
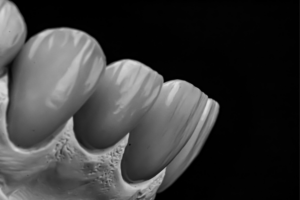
Bacterial Mechanisms Beta-lactamases and Target Alterations 🧬

Hidden in hospital wards and soil, bacteria adapt with astonishing creativity. Clinicians have watched routine drugs lose potency as pathogens sculpt molecular shields, and stories of treatment setbacks have become disturbingly common. Evolution here is fast, subtle, and sometimes dramatic.
One major route is enzymatic breakdown: beta-lactamases cleave the beta-lactam ring of ampicillin and similar agents, rendering them useless. Another is target alteration—mutations in penicillin-binding proteins reduce drug affinity, or bacteria thicken envelopes to lower penetration.
Resistance can spread via mobile genes, and outbreaks have Occured when diagnostics lag. Rapid testing, prudent prescribing, and novel inhibitors are needed to preserve options. The clinical puzzle is urgent: without action, everyday infections will again defy simple cures.
Role of Plasmids and Horizontal Gene Transfer 🔗
In a crowded hospital ward, tiny DNA circles hop between bacteria like secret notes, turning harmless strains into resistant foes. Plasmids can carry genes that neutralize ampicillin, and their movement often feels inevitable until human action slows it.
Conjugation, transduction and transformation are the highways of this genetic traffic; conjugative plasmids form bridges while bacteriophages and free DNA aid transfer across species. Such exchanges have occured in community and clinical settings, seeding outbreaks and complicating treatment.
Understanding plasmid ecology helps clinicians prioritise stewardship, rapid diagnostics, and infection control to limit spread. Preventing gene exchange is as much about behaviour and surveillance as about new drugs, stop the transfer, stop the resistance. Act now globally, urgently.
Global Trends Surveillance Data and Emerging Hotspots 🌍

Across continents, surveillance networks map rising resistance to common drugs such as ampicillin, revealing corridors where urban density, unregulated antibiotic use and weak health systems intersect. Data from WHO and national labs paints a mosaic: some regions show steady increases, others episodic spikes tied to outbreaks or agricultural antibiotic use. Timely reporting and standardized assays let epidemiologists track clones and resistance genes as they spread.
Hotspots often cluster where diagnostics are scarce and stewardship programmes are underfunded; improving laboratory capacity and data sharing can Acomodate earlier intervention. Innovative sentinel sites and genomic surveillance have uncovered transmission chains that were invisible to routine surveillance, enabling targeted interventions. Policymakers must invest in surveillance networks, cross-border collaboration, and public health infrastructure to slow dissemination and preserve effective drugs. Community engagement and open access to data are crucial for resilient regional response systems today.
Clinical Consequences Treatment Failures and Limited Options ⚠️
A simple urinary or bloodstream infection can become a fierce medical puzzle when standard drugs fail; ampicillin resistance turns routine care into a hunt for effective therapy. Clinicians face longer hospital stays, higher mortality risk, and the urgent need to escalate to broader-spectrum agents that may carry more side effects and cost.
Rapid diagnostics are essential to guide targeted therapy and avoid unnecessary use of last-line drugs. Teh shrinking antibiotic pipeline means clinicians often resort to combination regimens or older, toxic agents while research pursues new options to restore care.
Prevention Strategies Stewardship Diagnostics Vaccines and Hygiene 🛡️
In busy clinics and quiet homes alike, small choices shape resistance. When clinicians prescribe narrowly and patients complete courses, unnecessary exposures fall and labs can more quickly Recieve meaningful cultures that guide therapy.
Rapid diagnostics cut guesswork: point-of-care tests and stewardship protocols stop broad-spectrum use and preserve options like ampicillin for cases where they work. Vaccination programs reduce infections before antibiotics are even needed, a simple triumph of prevention.
Hygiene, handwashing and clean water are the everyday defenses that buy time for new tools; global surveillance and coordinated policy keep pressure on misuse and incentivize research. Collective effort, from wards to communities, makes containment realistic. Clinicians, public health and citizens all must continue to engage. PubChem: Ampicillin NLM Drug Portal: Ampicillin